genotyping is sometimes also undertaken for the
purposes of clinical epidemiology and hospital infec-
tion control (Pfaffer and Herwaldt 1997).
Acute phase response
The acute phase response is a group of nonspe-
cific, cytokine-mediated phenomena that occur in
response to inflammation (Gabay and Kushner
1999). As shown in Table 9.2, one or more compo-
nents of the response may be present as a conse-
quence of infection. Which components are present
is determined by the set of cytokines characteristi-
cally generated during the infection. Bacterial infec-
tions, for instance, typically cause a wide variety of
cytokines to be released, resulting in all three of the
classical components of the acute phase response:
fever, neutrophilia, and increased plasma concentra-
tions of the acute phase proteins.
Both the acute phase protein reaction and neutro-
philia have been used as markers for bacterial infec-
tion. The acute phase proteins, C-reactive protein
and fibrinogen (usually measured using the ESR),
are often increased in bacterial infection but the
specificity of these markers, as would be predicted,
is quite low.
The neutrophilia that occurs as part of the acute
phase response is due largely to the release of
mature neutrophils held in reserve in the marrow
sinusoids, but slightly immature cells, band neutro-
phils, may also be released. Neutrophilia is demon-
strated by an increase in the neutrophil count. The
neutrophil count is the concentration of neutrophils
in whole blood. The neutrophil count is often called
the
absolute
neutrophil count to distinguish it from
the neutrophil fraction as reported in a white cell
differential. Because neutrophils make up a large
fraction of the white cells in circulation, an increase
in neutrophil count usually produces an elevation in
the white cell count. Increased white cell counts are
not inevitable, however, and increased neutrophil
counts can be found in some infected patients who
have normal white cell counts (Ardron et al. 1994).
Neither the neutrophil count nor the white cell count
are highly sensitive markers of bacterial infection.
This is not surprising as the range of tissue damage
and extent of systemic response caused by
infections, even infections with the same pathogen,
vary so greatly among patients. The neutrophil
count may be somewhat more specific than the white
cell count in some clinical settings (Gombos
et al.
1998). Because band neutrophils may be released
as part of the acute phase neutrophilic response, the
measurement of the band neutrophil count has also
been used as a marker of bacterial infection (Novak
1993). The quantification of band neutrophils is
even incorporated into most automated blood cell
counters. Despite its appeal, the band neutrophil
count is no more reliable as a marker of infection
than is the neutrophil count (Bentley
et al.
1987,
Ardron
et al.
1994).
The finding of neutrophils in body fluids being
evaluated for bacterial infection quite reliably
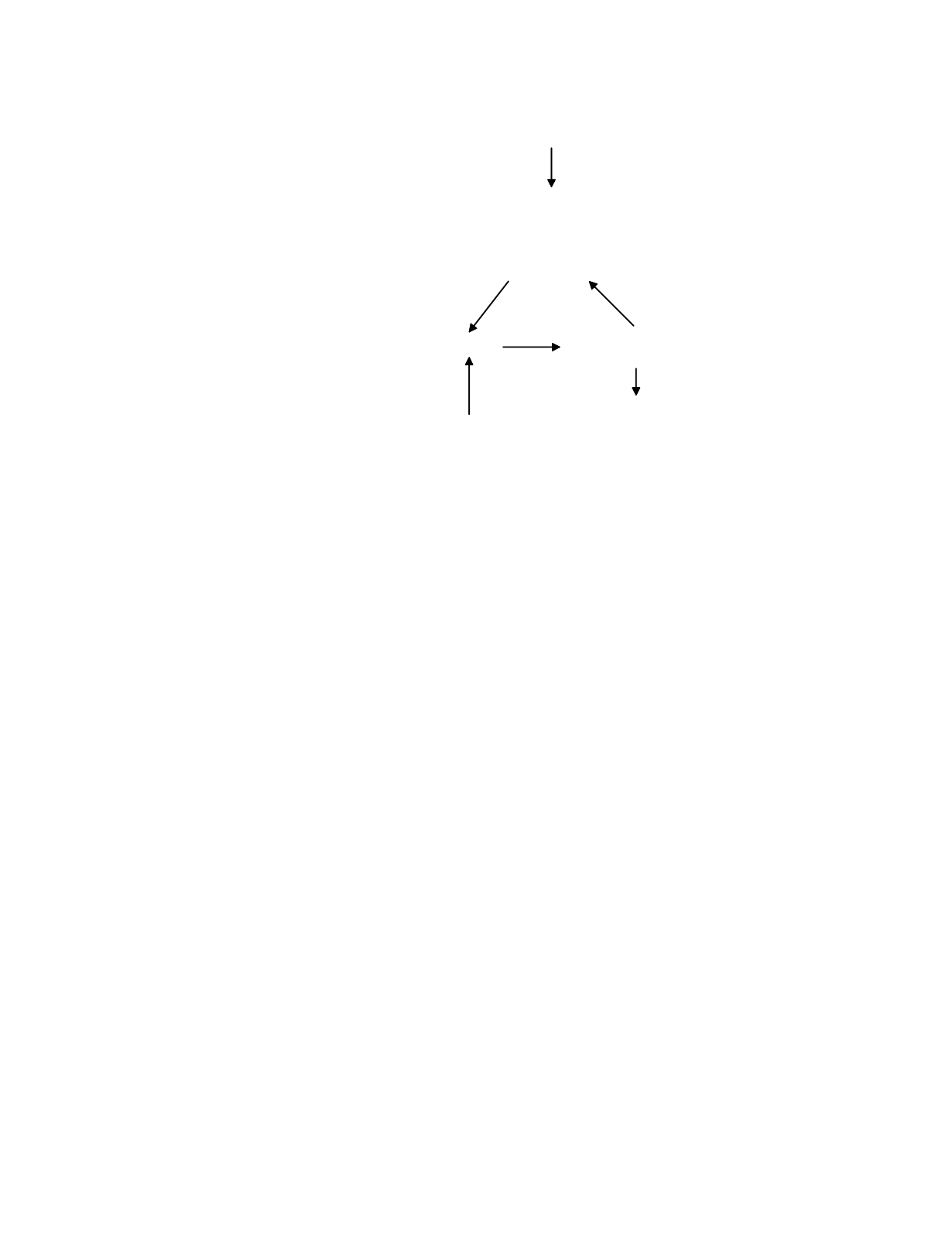
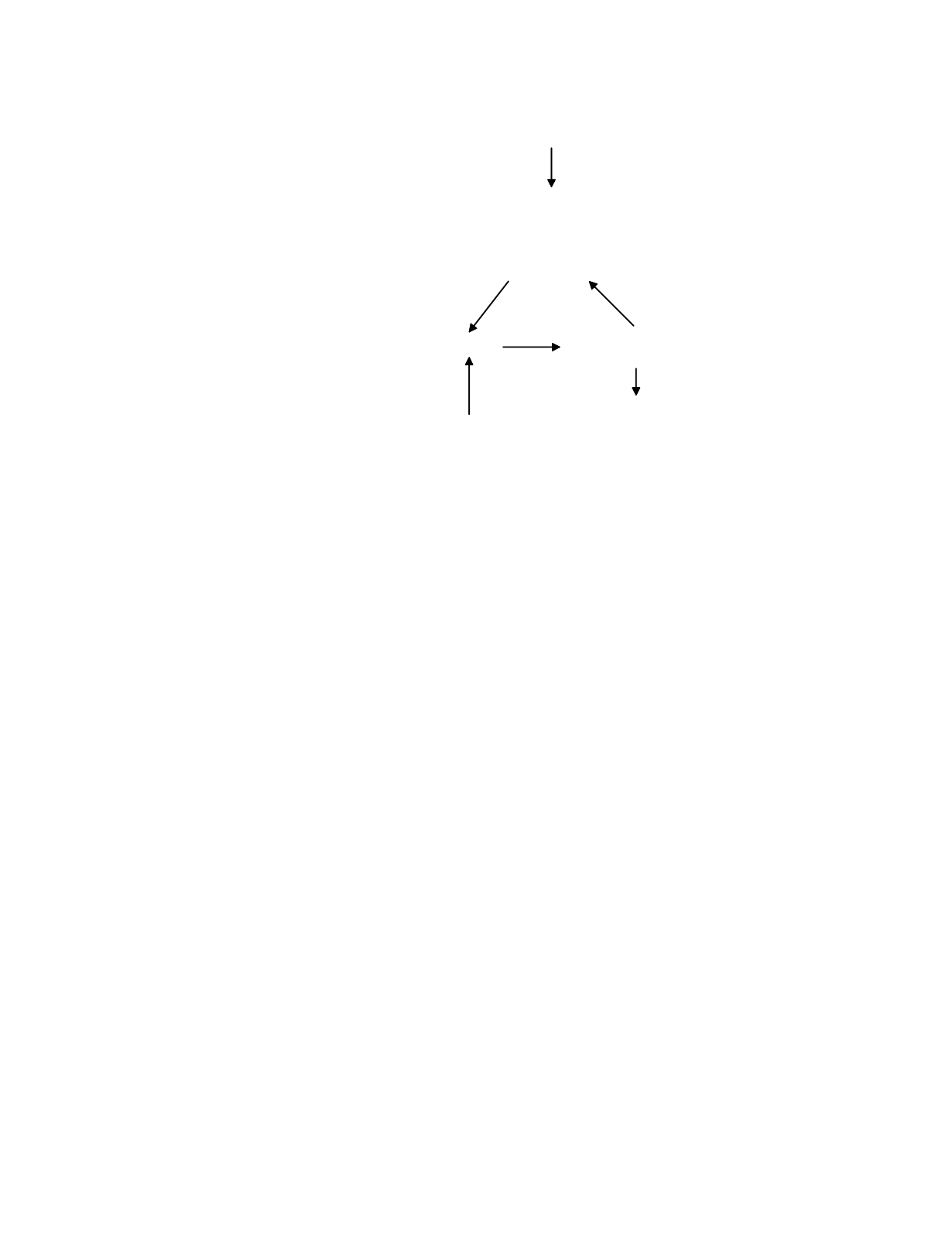
Tissue Injury
9-13
plasma
extracellular fluids
lymph
SITE OF
INFECTION
organism
proteins
nucleic acids
metabolic products
secreted products
LYMPHOID
TISSUE
antibodies
cytotoxic T cells
PLASMA AND
EXTRACELULAR FLUIDS
excreta
Figure 9.3
A model of the disposition of high specificity markers of infection.