serve as a marker of the disorder. Hyperparathy-
roidism, for example, leads to decreased renal
tubular reabsorption of phosphate. Renal phosphate
reabsorptive capacity therefore can, and indeed has,
been used as a diagnostic study in this disease.
The distribution of blood flow through the
vascular bed is a major determinant of the uptake of
oxygen by the lungs. This is because of the alveolar
structure of the lungs: capillary blood absorbs
oxygen from only one alveolus; if the blood supplies
an alveolus that is hypoventilated or if the blood is
shunted around the alveolus into the venous circula-
tion, oxygen uptake will be reduced. Normally,
autoregulatory mechanisms redistribute blood away
from hypoventilated alveoli and the degree of shunt-
ing is small. However, in the presence of pulmo-
nary disease, appreciably amounts of pulmonary
blood flow may pass through shunts (right-to-left
shunting) and the distribution of blood flow may be
impaired with overperfusion of hypoventilated
alveoli and reciprocal underperfusion of normo- and
hyperventilated alveoli (called, ventilation-perfusion
mismatch). The contribution of these two mecha-
nisms of oxygen hypoabsorption to a patient's
hypoxemia can be assessed by increasing the oxygen
content of the air inspired by the patient. This will
correct the impaired absorption due to hypoventila-
tion and therefore to ventilation-perfusion mismatch.
This maneuver will not reverse the hypoxemia due
to shunting. Because normally aerated blood is
highly saturated with oxygen, when unshunted
pulmonary blood is exposed to alveolar air with an
high oxygen content, the increase in oxygen carriage
in the unshunted blood is very small. Consequently,
the shortfall in the oxygen content in shunted blood
cannot be made up for by an increase in the oxygen
content of unshunted blood; the mixed pulmonary
venous blood will remain underoxygenated.
Finally, if the capacity of the blood to transport
a substance from its site of absorption depends upon
the substance binding to a protein in the blood, the
blood concentration of the transport protein will also
affect the absorption of the substance. Measurement
of the transport protein concentration is then an
important component of the evaluation of absorptive
function. For example, the uptake of oxygen in the
lungs is determined largely by the concentration of
hemoglobin in the blood as the oxygen transport
capacity of plasma is very small. So, the clinical
evaluation of oxygen transport must include
measurement of the blood hemoglobin concentration.
HOMEOSTATIC SYSTEMS
One of the fundamental activities of physiologic
systems is to maintain a constant internal environ-
ment despite perturbing stimuli. This is homeostasis
(from the Greek
homio
, similar or like, and
sta
, to
stand). Homeostasis most often is accomplished
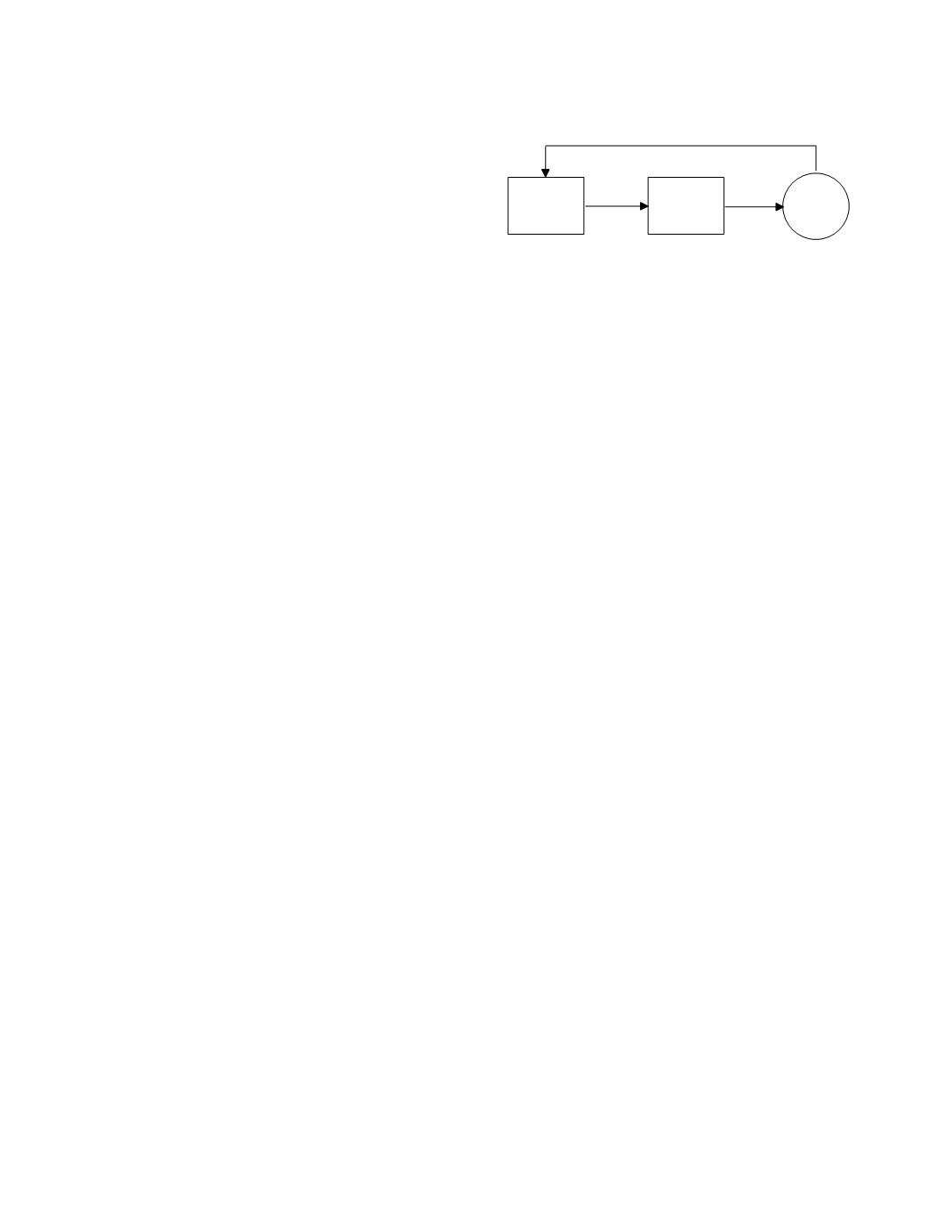
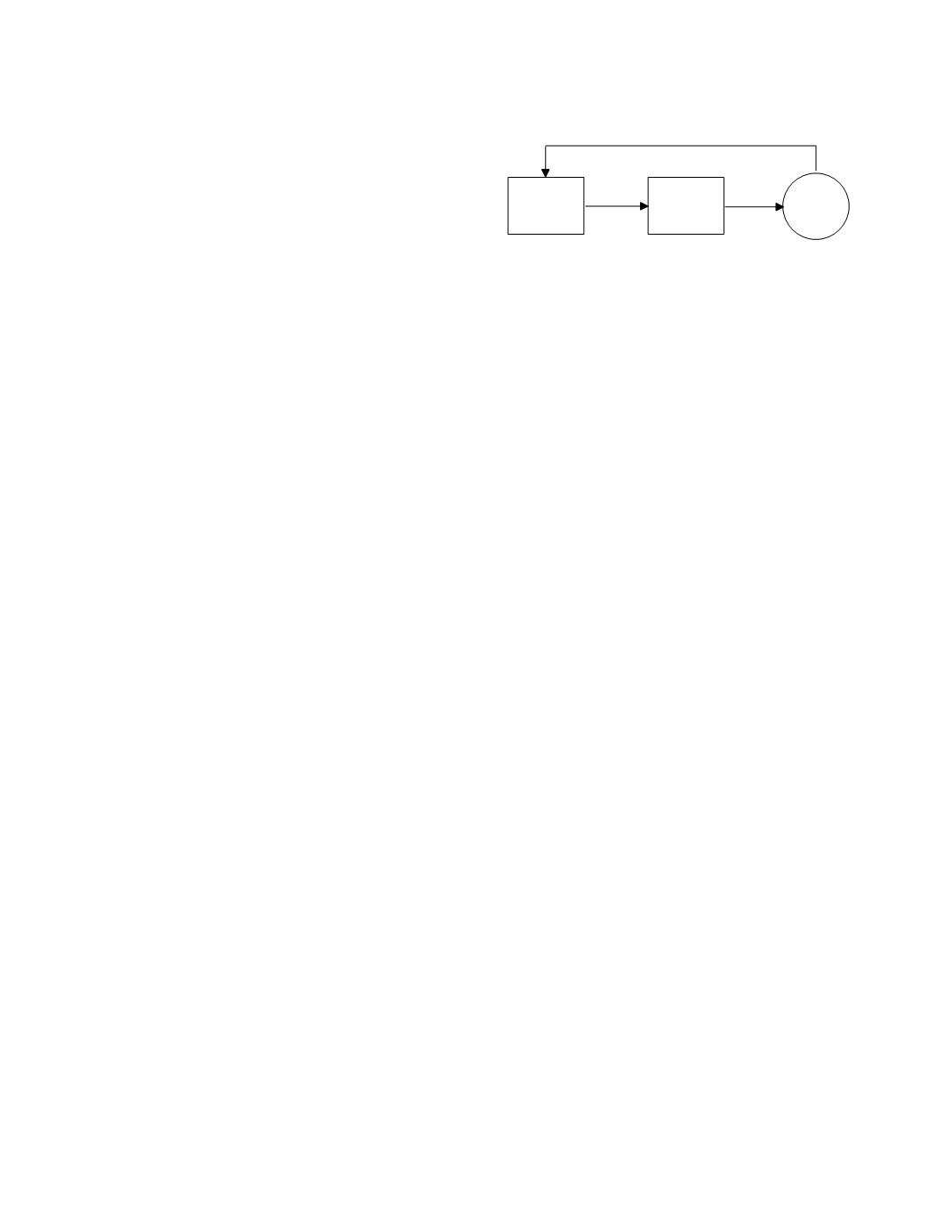
actively. Figure 7.6 illustrates the essential compo-
nents of active homeostatic regulation (Houk 1988).
A regular tissue controls the state of the target
process through the magnitude of an effector signal.
This signal is received by a biologic transducer,
most often an effector tissue, the cells of which
contain receptors for the effector signal. The regula-
tor tissue maintains a vigilant surveillance of the
target process. The magnitude of a feedback signal
from the process is monitored by sensors in the
regulator tissue. Alterations in the state of the
process as reflected in alterations in the feedback
signal initiate the corrective changes in the level of
the effector signal.
An example of such a homeostatic system is
found in the regulation of the plasma calcium
concentration. The regulator tissue is the parathy-
roid glands. The glands monitor the ionized calcium
concentration (the feedback signal) through a
calcium sensor. They secrete parathyroid hormone
(the effector signal) in response to the magnitude of
the feedback signal: high calcium concentrations
decrease parathyroid hormone secretion and low
concentrations increase it. The effector signal, i.e.
the hormone, acts through specific membrane recep-
tors in many body tissues (the effector tissues). In
the renal tubules, for instance, the binding of
parathyroid hormone to its cell-surface receptor
activates the cAMP intracellular messenger pathway
(the effect) leading to increased tubular reabsorption
of calcium (the target process).
The equilibrium state of a regulated process,
usually called the homeostatic set-point, is deter-
mined by the control response curve of the regulator
tissue and the effect response curve of the effector
Organ Function
7-6
Figure 7.6
A model of active homeostatic regulation.
regulator
tissue
effector
tissue
target
process
feedback signal
effect
effector
signal