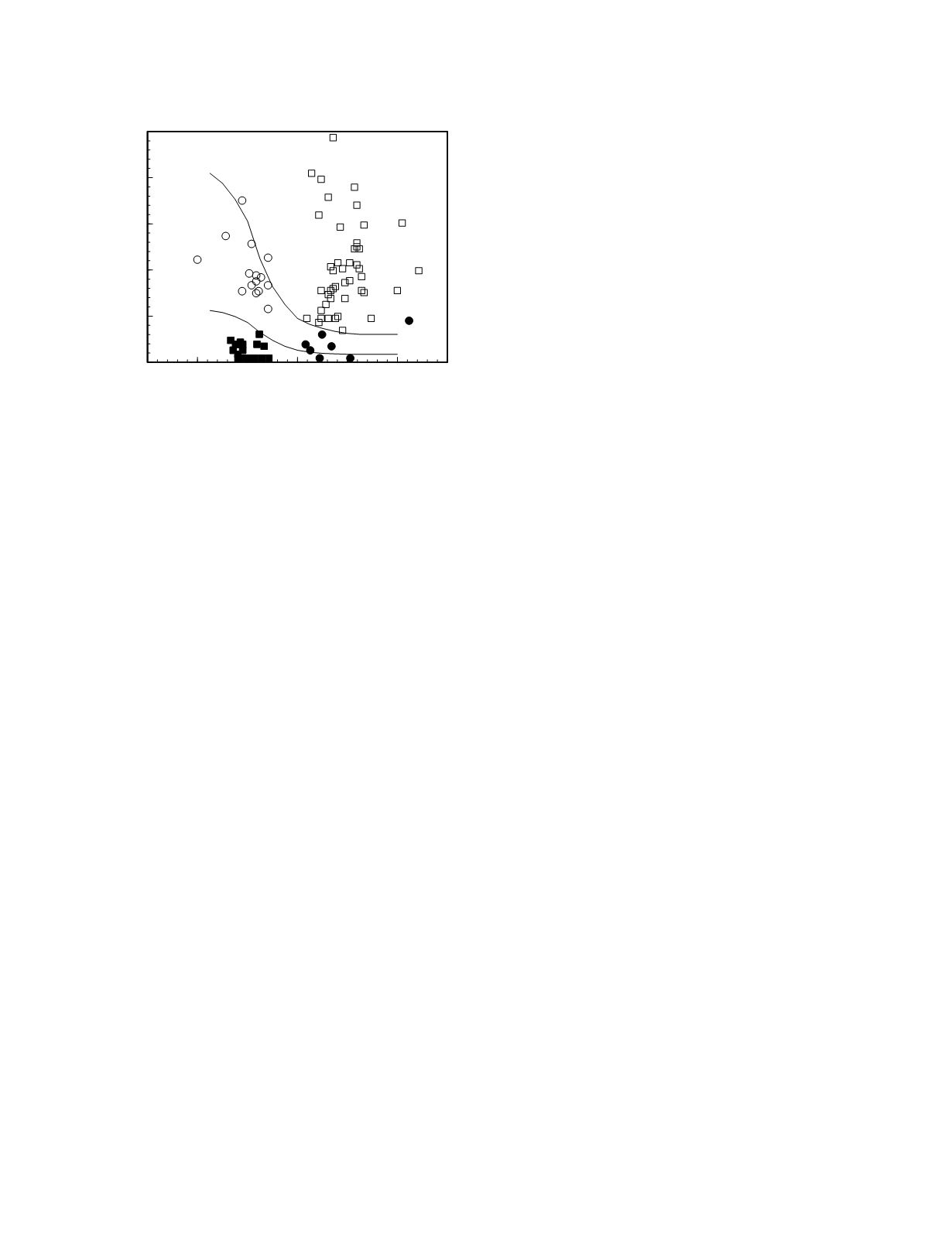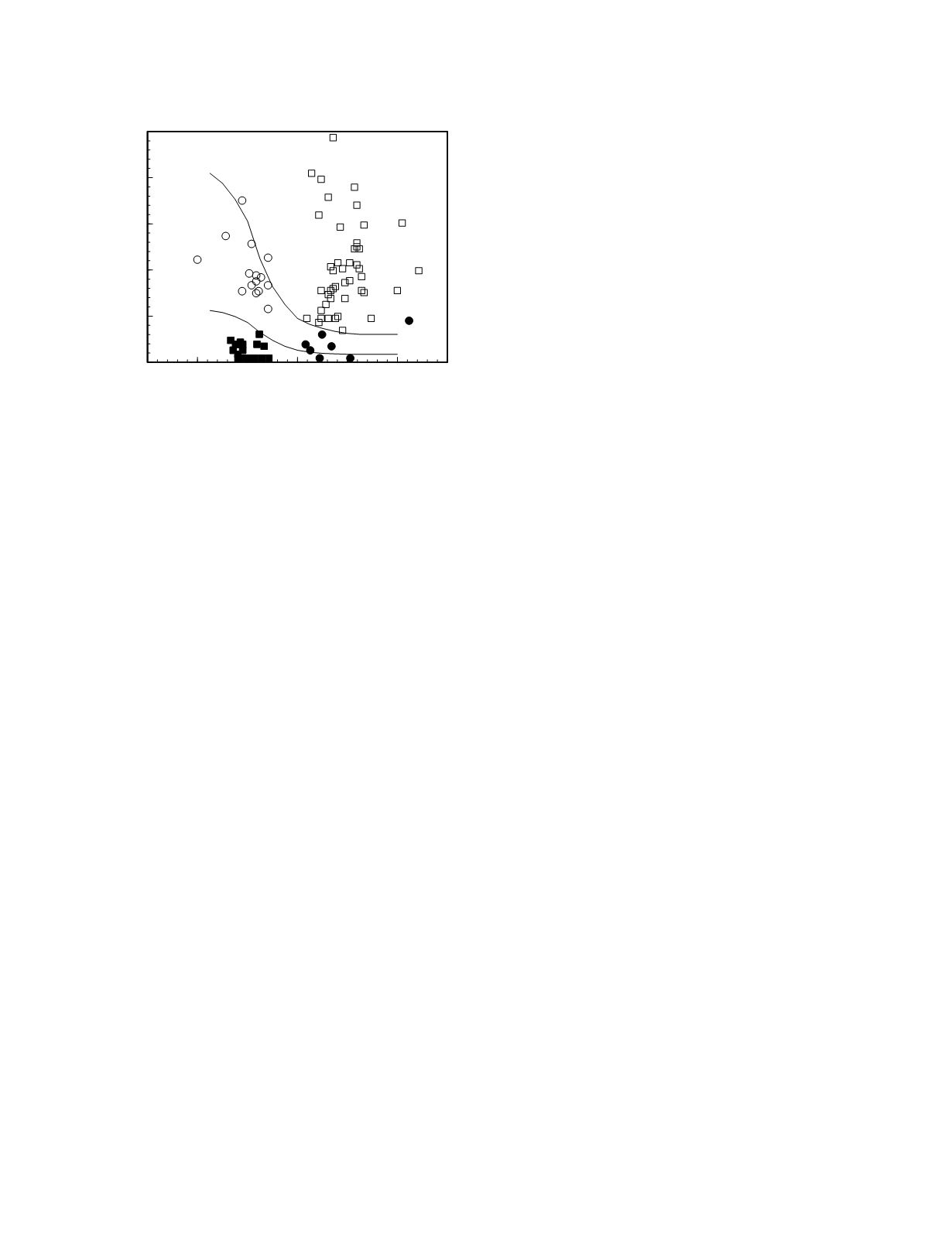
result pairs from patients with secondary disorders
of endocrine function will fall along the normal
control response curve while the result pairs from
patients with primary disorders will be located along
the normal effect response curve. Even though there
is considerable variability in the location of these
curves among individuals, clinical experience shows
that there is only a slight overlap of the diagnostic
regions. The diagnostic efficacy of this approach is
illustrated for parathyroid disease in Figure 7.11.
Here, the function marker is immunoreactive
parathyrin (iPTH) and the feedback signal is the
plasma total calcium concentration, although, of
course, the true feedback signal is the ionized
calcium concentration. Lepage
et al.
(1988) defined
the region characterizing the normal control response
curve from a study of 11 normal individuals made
hypercalcemic using CaCl
2
infusion and hypocalce-
mic using Na
2
EDTA infusion. Individuals with
paired calcium and iPTH concentrations in this
region have secondary calcium disorders because
their homeostatic set-points are consistent with a
normal control response curve. Patients with paired
calcium and iPTH concentrations outside of this
region have homeostatic set-points that could not
arise from a normal response curve; they, therefore,
have primary calcium disorders. The data from
these patients define the region characterizing the
normal effect response curve.
Effector tissue function is tested directly by
monitoring hormone effect following the administra-
tion of the hormone. If physiologic concentrations
of the hormone produces a typical response, the
effector tissue is functional. If the hormone fails to
evoke an adequate response, the function of the
effector tissue is impaired. Decreased functional
mass of the effector tissue is the most common cause
of diminished function. Less commonly, an
adequate effector tissue mass is present but it is
composed of cells with abnormal or sparse hormone
receptors, such as in nephrogenic diabetes insipidus,
or post-receptor-binding defects in cellular function,
such as in pseudohypothyroidism.
PROTEIN-BOUND TRANSPORT IN BLOOD
Many substances in the blood are transported
partly or completely bound to proteins. Oxygen and
some carbon dioxide is transported bound to intra-
erythrocytic hemoglobin and various plasma
constituents are bound to plasma binding proteins
(Table 7.1).
Blood constituents that have limited solubility in
plasma achieve much greater blood concentrations
when transported bound to a protein. This is the
vehicle function of protein binding. The transport of
oxygen is an example of this binding function.
The storage function of protein binding, in
which the binding of a blood constituent to a trans-
port protein results in a decreased passage of the
substance into the glomerular filtrate and thence the
urine, is one mechanism to reduce wasteful renal
loss of trace nutrients and thereby lower dietary
needs for the nutrients. The maintenance of body
stores of iron, for examples, is accomplished not
only by the transport of plasma iron as transferrin
but also by the protein binding of iron-bearing
hemoglobin and heme released into the plasma
following intravascular hemolysis. Urinary loss of
iron occurs only when the amount of hemoglobin or
heme released from a hemolytic episode exceeds the
binding capacity of their transport proteins. An
equally elaborate scheme for maintaining the body
stores of a trace nutrient exists for retinol (vitamin
A). Retinol binds with high affinity to the low-
molecular-weight protein, retinol-binding protein.
The pair then forms a complex with prealbumin, a
minor thyroxine-binding globulin. Unlike the
Organ Function
7-11
Figure 7.11
Diagnostic plot for the separation of disorders
of the parathyroids based on plasma total calcium concen-
tration and plasma immunoreactive parathyrin (iPTH)
concentration (redrawn from Figs 3 and 4, LePage
et al.
1988). The data shown came from hypercalcemic patients
with surgically proven primary hyperparathyroidism (open
squares) and various forms of secondary hyperparathyroid-
ism (filled circles), and hypocalcemic patients with primary
hypoparathyroidism (filled squares), and secondary hyper-
parathyroidism without renal failure (open circles).
1
1.5
2
2.5
3
3.5
4
Calcium (mmol/L)
0
10
20
30
40
50
iPTH (pmol/L)