than a study that is not offered at all. Alternative
studies that can be obtained in a timely fashion must
then be used instead.
Another and more frequent consideration in
ordering studies is the time that elapses between
requesting a study and receiving the result. If the
wait is short, a study can be ordered and the result
received and interpreted prior to requesting the next
study, if additional testing is indicated. This is
sequential test ordering. It is efficient because each
study ordered contributes to clinical care and is cost-
effective because the number of studies ordered is
minimized. If the turnaround time is long, however,
the patient's care is compromised by the cumulative
delay in obtaining study results occasioned by
sequential testing. In that case most or all of the
potentially useful laboratory studies can be ordered
together and the results interpreted
en masse
. This
is concurrent ordering. It is not efficient but, when
properly used, is cost-effective since the costs of
delayed care are minimized. Concurrent ordering
must not be confused with the indiscriminate order-
ing of laboratory studies by those who have the
misconception that the greater the number of studies
ordered, the greater the amount of information that
will be available for use in the care of the patient.
Remember, data is not always information! Infor-
mative study results contribute to the care of the
patient. Superfluous study results, at best contribute
nothing to the patient's care, often obscure informa-
tive results, and sometimes even misinform.
Lastly, clinicians must keep in mind that labora-
tory studies are costly. The financial burden of
medical bills, especially outpatient bills, is in no
small part due to laboratory charges. In addition,
much of the physical and psychological discomfort
experienced by patients as part of their medical care
is attributable to the invasive nature of most labora-
tory studies. Although it is not always possible, it is
important to include cost as a consideration in study
selection.
EXPRESSING LABORATORY RESULTS
Most laboratory studies are simply measure-
ments. The information requested is of the type
"How much, or many, of some analyte is present in
this specimen?" As such, these studies quantify the
analyte of interest. The level of quantification
achieved varies depending upon clinical needs and
the sophistication of the method of measurement.
Qualitative studies are characterized by binary
quantification. The analyte is reported as either
"present" or "absent." Semiquantitative studies
arrange study results into grades or categories.
Results may, for example, be reported as "absent /
trace / moderate / marked" or "zone I / zone II /
zone III." Quantitative studies use a scale of
measurement. The scale is graduated according to a
reference measurement, called the unit of measure-
ment. The value of a quantitative measurement
indicates how many multiples of the reference
measurement, or unit, are contained in the specimen.
SI Units
There exists an international system of units, le
Systčme International d'Unités (abbreviated SI),
advanced by the International Committee of Weights
and Measures as the system of units to be adopted by
all signatories of the Diplomatic Convention of the
Meter, 1875 (Lehmann 1979). From this system
there has evolved a recommended system of units
(Recommendations 1978 and 1984) to be used in
medicine (Dybkaer 1978a; Dybkaer 1978b; Siggard-
Anderson
et al.
1987). These recommendations are
the product of the Clinical Chemistry Committee of
the International Union of Pure and Applied Chemis-
try (IUPAC) and the International Federation of
Clinical Chemistry. They are supported by the
International Committee for Standardization in
Laboratory-based Medical Practice
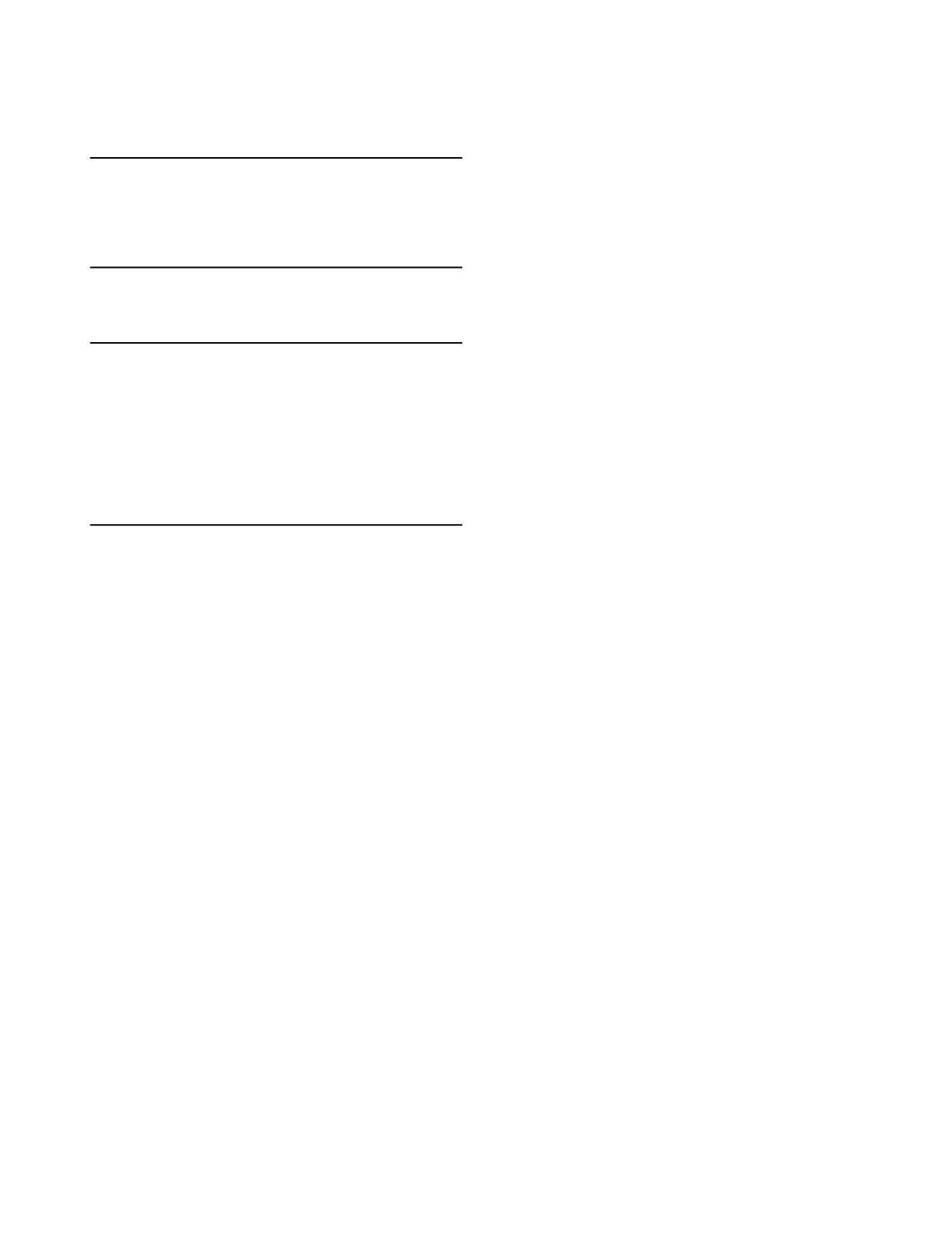
1-2
Table 1.1
Goals of Medical Care
1. Detect and quantify risk of future disease
2. Detect subclinical disease
3. Establish and exclude diagnoses
4. Assess disease severity and establish prognoses
5. Select appropriate therapy
6. Monitor disease progress and treatment effect
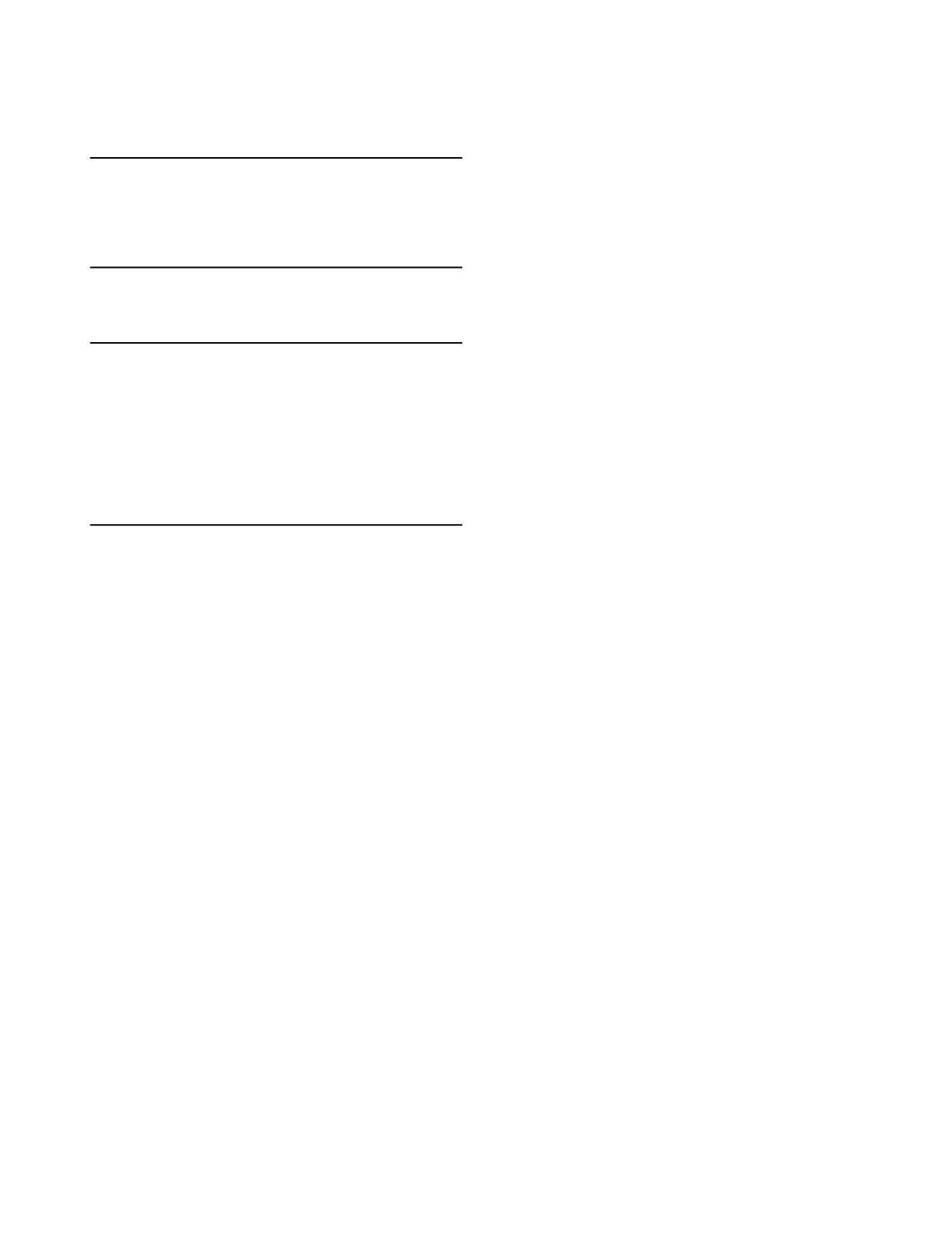
Table 1.2
Clinical Information Needs
1. Assess organ function
2. Assess metabolic activity
3. Assess macro- and micronutritional status
4. Detect and monitor neoplasia
5. Detect and quantify tissue injury
6. Detect and identify genetic disorders
7. Detect and identify immunologic disorders
8. Detect and identify infectious agents
9. Detect and identify intoxicants and poisons
10. Monitor therapeutic agents